Communities & Health Research
Raising the voice of communities for better, more inclusive health research
Rationale for doing this work
The Health Ambassadors felt that an important part of their role is to listen to what issues are important to communities and wanted to run a series of engagement activities to hear what communities felt they needed in relation health and social care – what are the issues of concern in communities, what do they think is missing.
Full Report
If you wish to read the full report of this work click here
Disclosure
We acknowledge that the data does not fully represent all communities and groups across BNSSG. While we have done our best to ensure inclusivity, we recognise there are limitations within this project.
Event Details
The health ambassadors are organizing three events as part of this project across BNSSG. Click here to learn more about the event details.
Methods of Engagement & Who We Spoke To
Everyone who participated in this work was paid for their time according to the NIHR guidance for Public Involvement at £25 per hour and travel expenses where required
We did the project in phases. First small group discussions ‘coffee mornings’, findings from these fed into the construction of a community survey where we asked people to rank what was most important and to comment on anything that they thought was significant or important to them and their communities. The survey was followed by a series of community workshops where we discussed priorities and invited people to create a collage about what is important to them related to health and wellbeing.
Coffee Mornings
We conducted a total of 10 ‘coffee mornings’ – these were small-group discussions with different communities, organised by Health Ambassadors. These sessions were mostly completed in-person, but three sessions were completed on-line. We organised these coffee mornings across Bristol, South Gloucestershire, and North Somerset.
Digital Surveys
We used the insights from the coffee morning sessions to inform the creation of an online community survey. Whilst we were aware of the many limitations of an online survey and the barriers to involvement it posed, we decided that a multi-method approach would create opportunities for more people to contribute to this work. The community survey was an online questionnaire, designed using Microsoft Forms, for anyone living in the BNSSG region. The Health Ambassadors shared this survey amongst their networks, and we also invited members of the BNSSG REN to complete and share the survey. People who completed the survey were anonymous, but had the opportunity to be entered into a prize draw for a £50 shopping voucher.
A total of 80 respondents, 76 were residents of Bristol, North Somerset and South Gloucestershire
We listed key interests and concerns raised by people in the coffee morning sessions under the categories of ‘General Health’; ‘Children’s Health’, ‘Women’s Health’, ‘Men’s Health’ and ‘Health and Research Workforce’ and asked people completing the survey to rank each in order of importance. We also asked them why they had ranked the issues in the order they chose and if they thought that anything was missing from the lists.
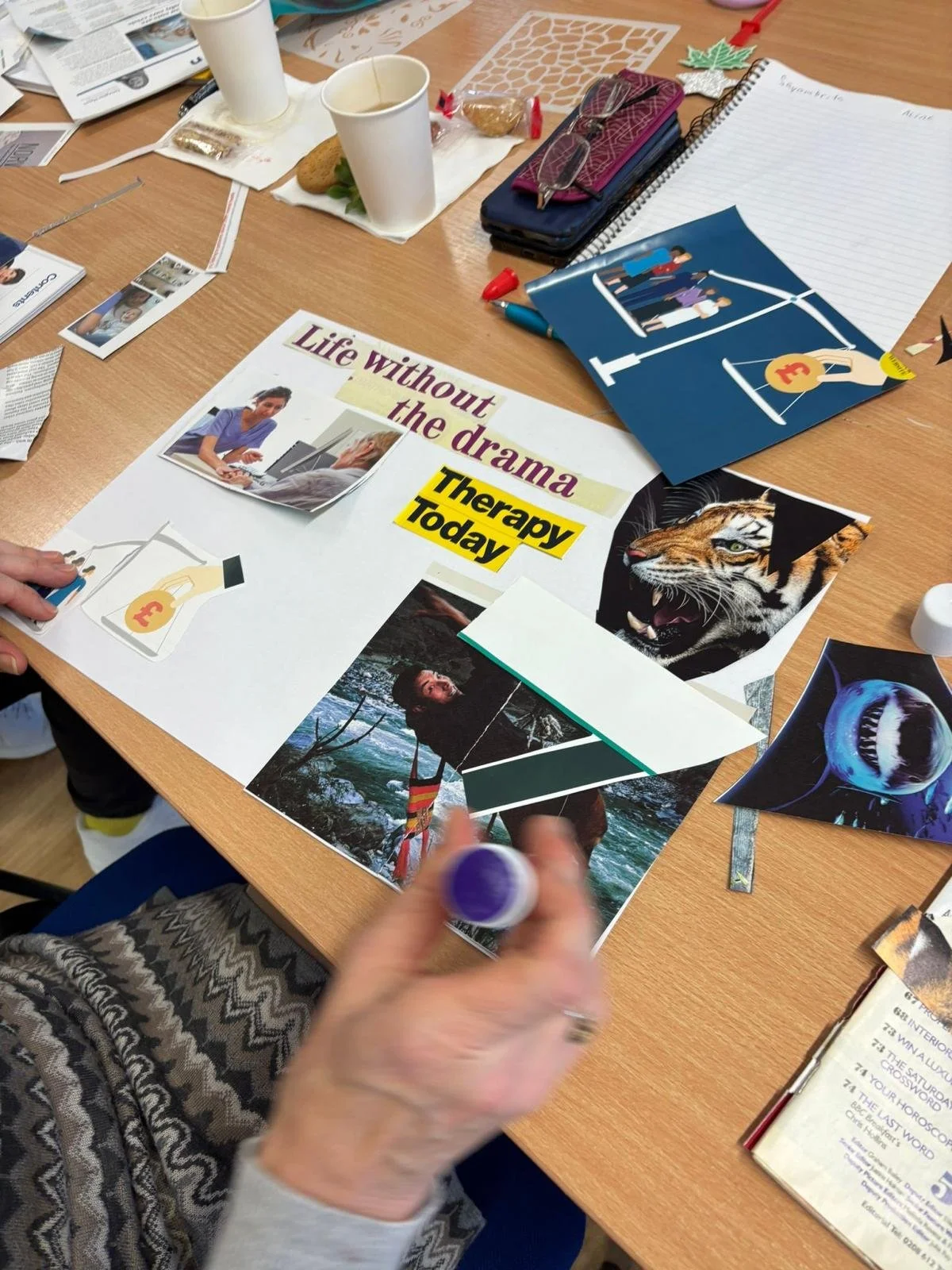
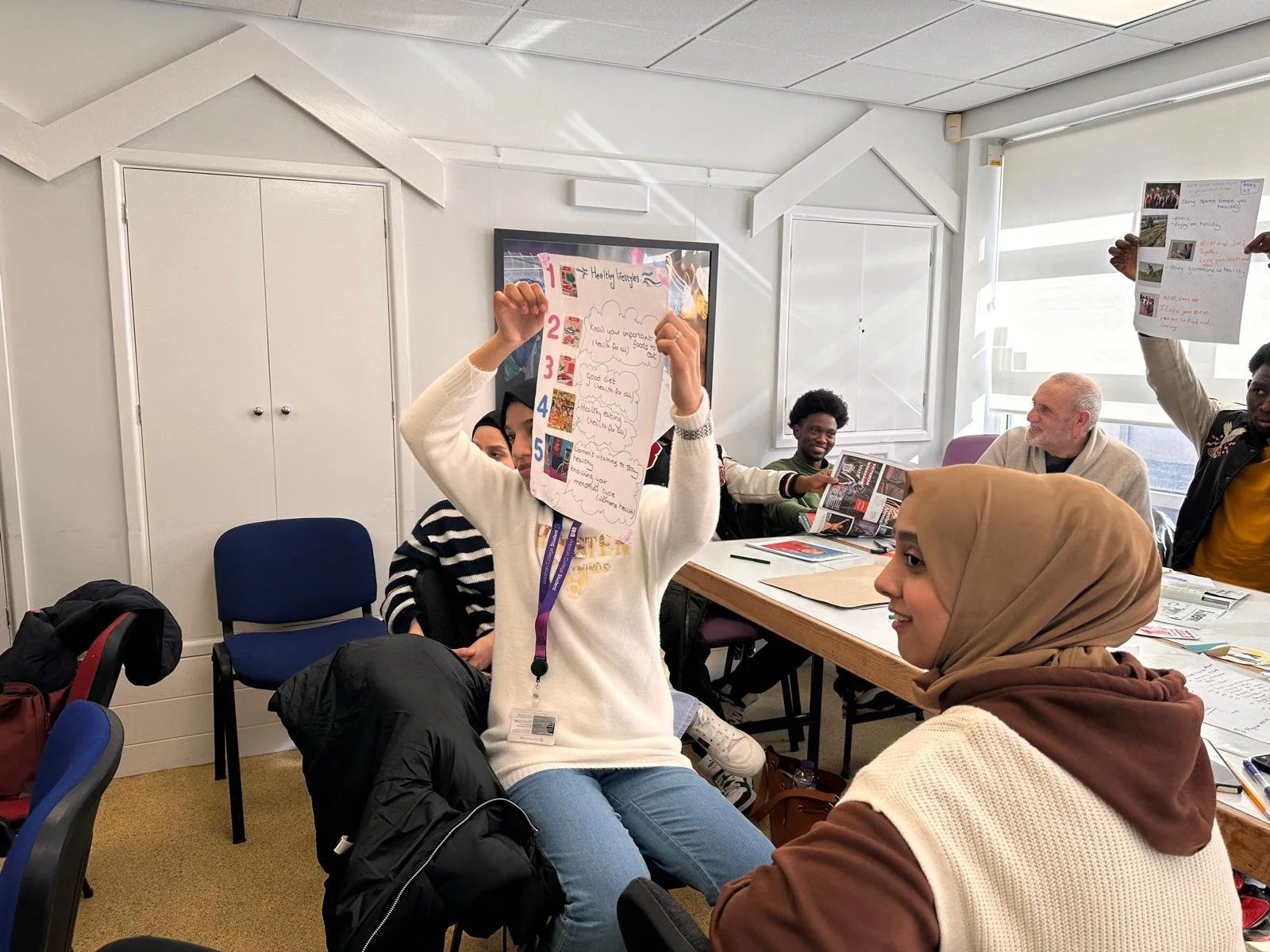
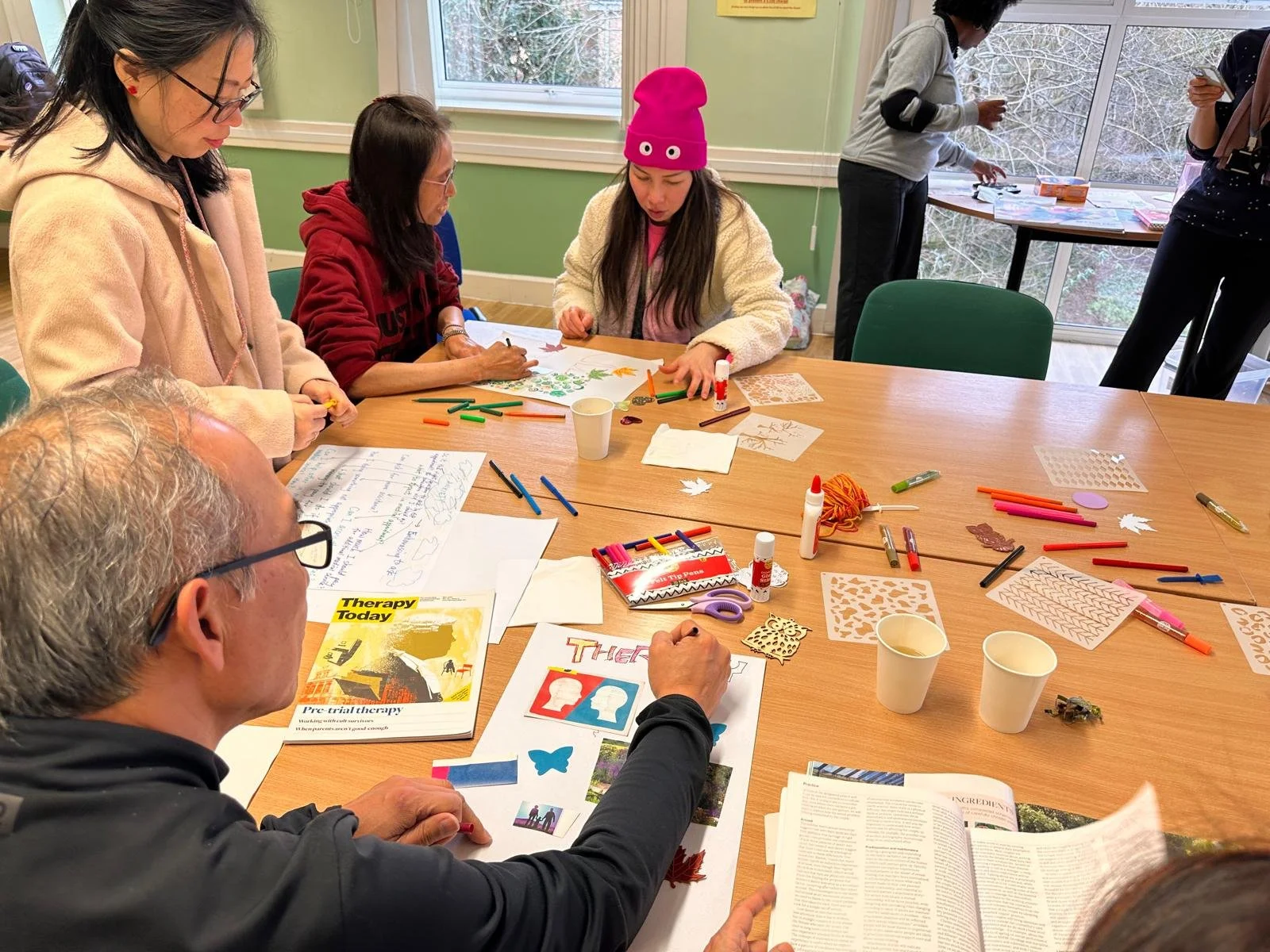
Creative Workshops
To explore community concerns further, we ran a series of creative workshops across the BNSSG region. During these sessions, individuals were first asked to select key priorities and consider solutions and potential research that could address these. Second, individuals were asked to create a collage using a mixture of art materials provided to explain a priority or concern that was important to them – they could complete this activity either individually or in groups.
We collected discussions through a combination of note-taking, audio recording, and collation of all the created collages.
Participants characteristics
Bristol (Women) – 19 participants, ages 22–7
Ethnicities: Eastern European, African Caribbean, Pakistani, Black British, Asian, Afghan, Indian Caribbean, Hong Kong, Middle Eastern, Mixed Race
Bristol (Men) – 14 participants, ages 20–70
Ethnicities: British Pakistani, Indian, African Caribbean, British Ghanaian African
South Gloucestershire (Mixed group) – 8 participants (2 men, 6 women), ages 30–57
Ethnicities: White British, Eastern European, Black British, Turkish, Somali
North Somerset (Mixed group) – 17 participants (9 men, 8 women), ages 17–68
Ethnicities: Afghan, Sudanese, Syrian, Black British, West Indian, Dual Heritage, Filipino, African, Brazilian/English, Moroccan, Ethiopian, Black African
What are the priorities of communities? !!
It’s difficult to summarise all the priorities, recommendations and themes that have emerged from our work in these pages. For a full understanding of the location-based and gender-based themes and priorities, please refer to the report.
Access to Healthcare
GP Access: Long waits, cancellations, lack of continuity, and difficulty getting appointments.
Dental Care: Lack of available NHS dentists for both adults and children.
Mental Health Services: Long waiting times and limited culturally appropriate support.
Specialists: Delays in referrals and communication breakdowns.
Receptionists as Gatekeepers: Many described them as rude or obstructive, discouraging people from seeking care.
System Complexity: Especially challenging for migrants, refugees, and older adults unfamiliar with the NHS.
Language & Digital Barriers: Translation issues and unfriendly online booking systems limited access.
Fear & Hesitation: Embarrassment, anxiety, and fear of bad news or being judged stopped people from seeking help.
Doctor–Patient Relationships
Short Appointments: People felt rushed and not listened to.
Communication Issues: Doctors seemed disengaged, focused on screens, and unaware of patients’ history.
Continuity of Care: Patients wanted to see the same doctor consistently to build trust.
Trust and Fear: Some feared being judged or removed from GP lists if they complained.
Cultural Competency: Lack of understanding of cultural backgrounds, leading to feelings of bias and marginalisation, especially among Black and minority ethnic women.
Mental Health
Central Concern: Deeply connected to physical, social, and cultural wellbeing.
Stigma: Strong in some communities, especially among older generations and men.
Access Issues: Long waiting times and lack of culturally appropriate or language-accessible support.
Limited Human Connection: Talking therapies often felt scripted and impersonal.
Desire for Community Support: Preference for peer groups, safe spaces, and social activities (e.g., exercise, nature, creative outlets).
Prevention and Healthy Living
Desire for Early Intervention: People want to take control before illness develops.
Barriers: Unaffordable gyms, cheap fast food, lack of access to green spaces.
Cultural Relevance: Health messaging and lifestyle advice often don’t reflect people’s cultural realities.
Need for Systemic Support: Calls for stronger government regulation, community-based initiatives, and better promotion of preventive services.
Systemic Concerns
Overloaded NHS: Understaffed, underfunded, leading to poorer outcomes.
Rise in Privatisation: Anxiety that healthcare is becoming unaffordable and profit-driven.
Medical Tourism: Some travel abroad for treatment due to lack of trust and access in the UK.
Community Recommendations !!
It’s difficult to summarise all the recommendations and themes that have emerged from our work in these pages. For a full understanding of the location-based and gender-based themes and priorities, please refer to the report.
Although the workshops weren’t explicitly focused on healthcare access, this issue came up repeatedly across all groups. People highlighted the importance of being seen by healthcare professionals when you need to be seen (i.e. not delayed).
Improving access:
Simplify access and reduce gatekeeping at GP surgeries.
Provide multiple booking options: in-person, phone, and online.
Expand walk-in or drop-in community clinics.
Increase awareness of what services are available and how to use them.
Building Trust & communication:
Ensure continuity of care with the same GP where possible.
Train receptionists and clinicians in empathy and communication.
Increase cultural competency training for healthcare professionals.
Strengthen trust between patients and doctors through better engagement
Holistic, Person-Centred Care:
Treat patients as whole people, not isolated symptoms.
Integrate physical, mental, and social care
Offer more time in appointments
Include non-medical options like lifestyle advice, exercise and community-based therapies
Expand community-based services:
Drop-in centres, peer support, outreach.
Mental Health:
Make culturally sensitive MH services more available.
Reduce waiting times for support
Promote community-led peer support and group activities
Improve education & open conversations around MH to reduce stigma
Prevention & Lifestyle Support
Invest in early intervention & education
Make health food & exercise opportunities more affordable and accessible
Provide culturally tailored health promotion
Priorities prevention in national and local health strategies
What is Next?
This project is just the beginning; there is still much more work to be done. Our next step is to ensure that the voices of our communities are heard by policymakers, local councils, healthcare professionals, and researchers. We are committed to sharing our findings widely and making sure that the insights gathered lead to real change.
We will also return to the communities who took part to share how their voices have shaped our work and the actions that followed. Together, we’ll continue building stronger, more inclusive connections between research and the people it serves.
The artwork was created based on themes from our community conversation.
Click here to download
Artist : Sevilay Kaya

The artworks produced during our workshops.































Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it's the only thing that ever has.” — Margaret Mead
This work has been funded by NHS England via the BNSSG Diverse Research Engagement Network (REN) and the National Institute for Health and Care Research: Applied Research Collaboration West (NIHR ARC WEST), Health Protection Research Unit Evaluation (HPRUE) and Behavioural Sciences & Biomedical Research Centre.